Step 1 Understand and Complete Your Advance Directives
Helpful information to get you started
ARE YOU READY TO SERVE AS A HEALTH PROXY OR POWER OF ATTORNEY?
UNDERSTANDING ADVANCE DIRECTIVES
Ask Abby
If you are 18 or older, you are at risk of losing the ability to make your own healthcare decisions — unless you have signed a form that protects you if you are ever unable to make your wishes known.
" When I got sick and was away at school, my mother was able to get information because I carried a form with me that she is my medical power of attorney." — A Student
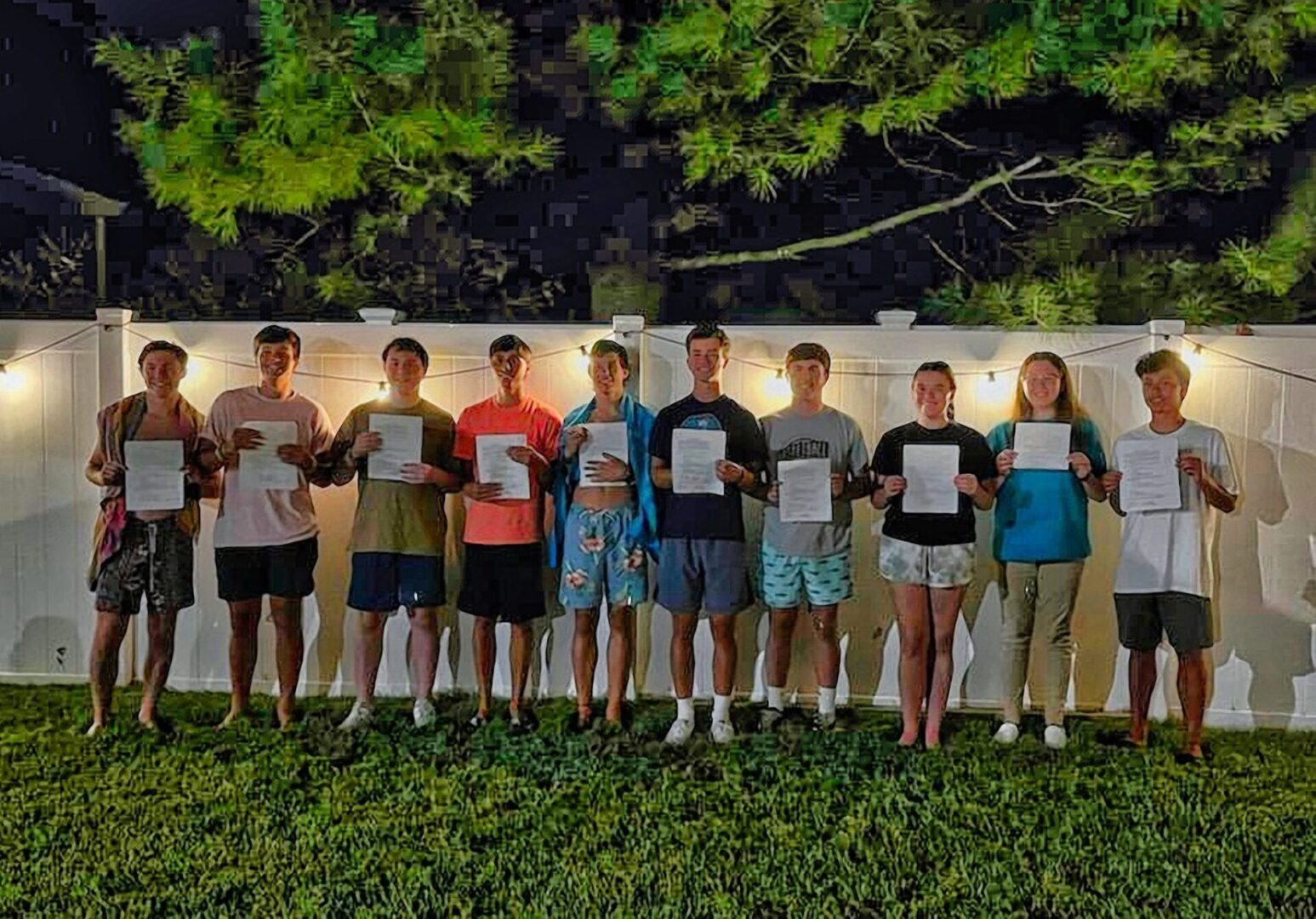
(Above) Youth Complete Healthcare Proxies Before Heading to College
These high school seniors — all childhood friends — are about to head off to college. But they used the opportunity of a farewell party to take an important step as they embark on life as adults: they all completed their healthcare proxies (Step #1 of TakeCHARGE: 5 Steps to Safer Health Care), designating someone to make medical decisions on their behalf should they ever, due to a medical condition, be unable to communicate their wishes. Congratulations! Learn more here www.TakeCHARGE.care
Advance Directives - Talking Points
Advance Directives allow a person who is unable to speak for him/herself to assert their right to make informed decisions by authorizing a trusted person to make decisions on their behalf.
Can you think of any situations in which an advance directive is needed?
Your child turns 18 and becomes unconscious or stops breathing (due to a choking incident, a car accident, a swimming accident, a sports injury, intoxication, etc…). Will the hospital/ER share confidential information with you about your adult child? Who will make critical decisions about urgent care?
A young adult goes away to college (near or far) and has a medical emergency that requires urgent medical care. Who makes decisions if he/she cannot?
A chronic illness or condition causes a decline in cognition (dementia, Parkinson’s Psychosis, a severe infection, Schizophrenia, Psychotic episode, etc..). Who decides on treatment options and care plan decisions?
A cancer patient is terminally ill and becomes unable to make decisions about his/her care. Who has the authority to make decisions on his/her behalf?
In each of the above situations, who knows the patient’s preferred wishes and is authorized to have the medical team carry them out?
It is important that you take the time to discuss these issues with your doctor and/or family, if appropriate, to make sure your wishes are known and you understand your responsibility and authority to carry out an advanced directive.
What Does a Healthcare Surrogate or Proxy Do?
A healthcare surrogate or proxy is a person designated by a family member or friend to make their medical decisions for them if they cannot speak for themselves or are not able to make their wishes or preferences known. The person may be incapacitated temporarily, for example after an accident or while under anesthesia or sedation during surgery. They may be affected by a permanent condition such as dementia or at the end of life with incurable cancer. Ideally a person shares their beliefs and preferences in advance as they go through the process of choosing a surrogate or proxy and completing the form which makes their choice clear for the medical team. This conversation may also occur at the time of injury, illness, or when the person is diagnosed with a life-threatening condition.
Discuss Ahead of Time
The person's medical condition and preferred treatment options
The person's preferred medical team and hospital
Review the person's medical chart together if appropriate
Access to and approval for release of the person's medical records
Requesting and coordinating second opinions or outside medical care
Preferred family, friends, and faith leader for support
The conversation need not be about death and dying. It is about beliefs and preferences. People who do not want to discuss dying may see this as an opportunity to explain what they would want if a choice must be made when they are not able to communicate for themselves. The surrogate will be expected to know the person’s wishes and approve or decline:
Types of medical care including experimental intervention, medicines, or surgery
Blood transfusions
Life-support treatments including feeding and mechanical ventilation
Pain management even if it may shorten their life
Where the person will receive care and treatment, possible transfer to another hospital, or state, or to a nursing home or hospice facility
Whether or not to allow organ donation
More Questions for the Conversation
“I hope we never have to know this, but do you want to donate your organs?” or “How do you feel about organ donation?”
“If you had a brain injury that left you with very limited functioning, would you want tube feeding or breathing machines to keep you alive?”
“I know this is unlikely, but if the operation shows an unexpected problem which could affect your fertility, would you rather the surgeon take care of it while they are in there? Or stop and wake you up to allow you to decide what you want done in a later operation?”
These are just a few examples of the wide variety of topics that may be discussed by a person and their healthcare surrogate or proxy, depending on the circumstances. Sharing your own thoughts during the conversation might be helpful. There are online and in-person programs and services available to assist any person or family exploring the considerations and choices involved in designating a healthcare surrogate and completing Advanced Directives.